Abstract
Background:
Monoclonal gammopathy of undetermined significance (MGUS) is a diagnosis that is often incidentally made after a serum protein electrophoresis (SPEP) is ordered as part of the evaluation for multiple nonspecific symptoms and is often ordered by non-hematologists. Currently, there is a lack of guidance regarding the extent of evaluation and follow-up required for these patients.
Objective:
Determine whether the risk stratification of the abnormal SPEP predicted progression to multiple myeloma (MM) or other lymphoplasmacytic malignancies (LPM) and could act as a guideline for appropriate follow-up in attempts to provide evidence-based, higher value care.
Design:
A retrospective review was performed of patients referred to the county hematology clinic for an abnormal SPEP from 2012 to 2019. The SPEP results were then risk-stratified and individual patient charts were reviewed to determine the symptomatology present at the time it was ordered, as well as the clinical course of the patients over time.
Main Measures:
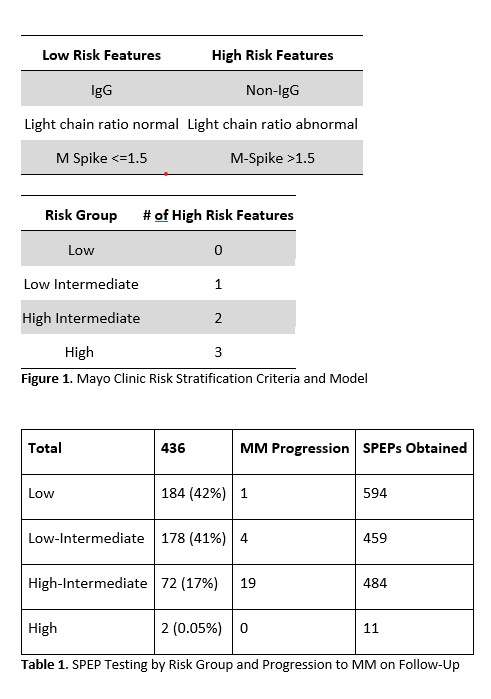
Patients were stratified into low, low-intermediate, high-intermediate, and high risk groups for progression to MM based on the Mayo Clinic criteria. Additional information was also analyzed including the number of SPEP tests per patient, the indication stated for ordering the SPEP, and the presence of symptoms that are associated with MM at the time the SPEP was ordered, including anemia, renal failure, hypercalcemia, and bone lesions (commonly known as "CRAB symptoms").
Results:
We abstracted data from 436 patients referred to the hematology clinic associated with a large county hospital system for an abnormal SPEP. The most common documented reasons for SPEP testing were increased creatinine (35%), protein gap (12%), and decreased hemoglobin (11%). Of these patients, 24 (5.5%) developed MM, 19 of whom were stratified into the high-intermediate risk group. More than a thousand SPEP results were obtained in the low and low-intermediate risk groups with only 5 patients diagnosed with MM. In the high-intermediate and low-intermediate risk groups, between 2-3 SPEP tests were performed prior to making the diagnosis of MM. In the low risk group, 6 SPEP tests were performed prior to reaching the MM diagnosis. Among the 5 patients in the low and low-intermediate risk groups who developed MM, all 5 had one or more of the CRAB symptoms at the time of the initial SPEP.
Conclusion:
Of the patients with MGUS who progressed to MM, approximately 80% were in the high-intermediate risk group. Of the remaining patients who progressed to MM from the lower risk groups, all had one or more of the previously mentioned CRAB symptoms, a higher percentage compared to the low and low-intermediate risk groups overall. In the absence of symptomatic disease, there is insufficient evidence to support serial SPEP testing in the lower risk patients. The use of evidence-based risk stratification may minimize unnecessary testing and hematology referrals while resulting in significant cost-savings and higher value care.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal